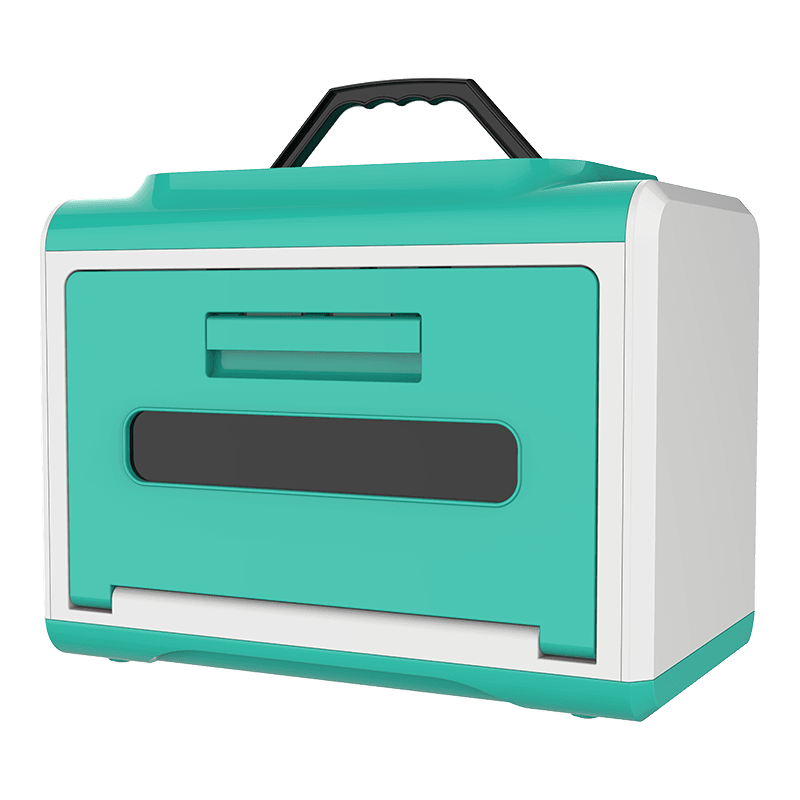
Medical disinfection cabinets are sterilization equipment used exclusively in medical institutions. They use physical or chemical methods to kill pathogenic microorganisms (bacteria, viruses, fungi, etc.) on medical devices, rendering them sterile (sterilization level) or meeting safe use standards (disinfection level). They are regulated as Class II medical devices.
Content
1. Core Sterilization Principles
High-Temperature and High-Pressure Steam Sterilization (Most Commonly Used)
Principle: Saturated steam at 134°C, 205 kPa, for 5-15 minutes
Applicable to: Metal instruments, rubber products, and other heat-resistant items
Representative Equipment: Pulsating Vacuum Sterilizer
Low-Temperature Plasma Sterilization
Principle: Hydrogen peroxide vaporizes and ionizes to produce plasma
Advantages: Operating temperature of 40-50°C, suitable for electronic devices
Ethylene Oxide Sterilization
Features: Strong penetrating power, suitable for complex instruments
Limitations: Requires a 12-hour ventilation and desorption period
UV/Ozone Disinfection
Applications: Surface disinfection (e.g., endoscope cabinets)

2. Clinical Use Guidelines for Medical Disinfection Cabinets
- Pretreatment Phase
Instrument Cleaning
Immediately soak in a multi-enzyme cleaner after use (≤ 1 hour)
Luminal instruments should be rinsed with a high-pressure water jet (pressure ≥ 0.4 MPa)
Complex instruments should be disassembled into their smallest components
Drying Inspection
Wipe metal instruments with anhydrous ethanol to prevent rust
Visually inspect for residue (with magnifying glass)
Joints and teeth should be cleaned with a dedicated brush
- Loading Requirements
Instruments should be thoroughly cleaned and decontaminated
Packaging materials should be breathable (e.g., Tyvek paper and plastic bags)
Loading capacity should be ≤ 80% of the cabinet volume
- Monitoring System
Physical Monitoring: Printed temperature/pressure curves
Chemical Monitoring: Color change indicator cards
Biological Monitoring: At least once a week (Bacillus stearothermophilus test)
3. Key Points for Medical Disinfection Cabinet Maintenance
- Daily Maintenance (Daily/Per Shift)
Surface Cleaning
Wipe the exterior with a neutral detergent (do not use chlorine-containing disinfectants)
Disinfect the control panel with a 75% alcohol pad (avoid liquid penetration)
Basic Inspection
Check the integrity of the door seal (no cracks or deformation)
Confirm that the emergency release is functioning properly
Record operating parameters (temperature/pressure fluctuation range)
- Periodic Maintenance
|
Maintenance Items |
Frequency |
Operating Standards |
Test Tools |
|
Cavity Deep Cleaning |
Weekly |
Descaling (soak in 5% citric acid solution for 30 minutes) |
Endoscope |
|
Filter Replacement |
Monthly |
HEPA filter efficiency ≥ 99.97% |
Particle Counter |
|
Seal Lubrication |
Quarterly |
Apply medical silicone grease (thickness 0.1-0.3mm) |
Thickness Gauge |
|
Safety Valve Calibration |
Annually |
Opening Pressure ±5% of Rated Value |
Pressure Calibrator |
|
Vacuum Pump Maintenance |
500 Hours |
Replace ISO VG32 Special Oil |
Oil Quality Tester |
- Key Component Maintenance
Steam Generator System
Drain excess water daily (to prevent scaling)
Test conductivity monthly (≤15μS/cm)
Disassemble and inspect electrode rods quarterly (scale accumulation requires polishing)
Control System
Set backup parameters (at least two backups)
Check sensor calibration (temperature sensor error ≤±0.5°C)
Piping System
Inspect hoses for aging (cracks/expansion require immediate replacement)
Verify steam trap function (discharge ≤30ml/minute)
4. Frequently Asked Questions (FAQ) about Medical Sterilizers
Basic Usage Questions
- What is the difference between medical and household sterilizers?
Medical sterilizers must comply with medical device management regulations (such as YY/T 0734) and achieve sterilization effectiveness (kill rate ≥ 99.9999%). Household sterilizers, on the other hand, only meet general disinfection standards and cannot be used for medical device processing.
- Why should instruments be cleaned before use in a sterilizer?
Organic residues (such as blood and protein) can hinder the penetration of sterilizing agents, resulting in sterilization failure. Thorough cleaning is a prerequisite for sterilization.
- What should I do if there is a sudden power outage during operation?
Immediately turn off the power. After power is restored:
Check whether the program is automatically saved.
If the interruption occurred during the sterilization phase, re-sterilize.
Record the incident and report it to the Equipment Department.
Sterilization Effectiveness Issues
- What does uneven color change on the chemical indicator card indicate?
Possible causes: Insufficient steam saturation, overcrowded loading, expired indicator card. Equipment parameters should be checked and retested, and biological monitoring verification should be performed.
- What should be done if a positive biological monitoring result is detected?
Immediately decommission the equipment and recall all items from the same batch. Check the sterilization process parameters, biological indicator validity, and equipment performance, and maintain written records.
- What should I do if water stains appear on instruments after sterilization?
This may be due to incomplete drying or water quality issues. Extend the drying time and use purified water. If the condition is severe, re-clean and sterilize.
Maintenance Issues
- What precautions should be taken for daily cleaning?
Use a neutral detergent.
Avoid liquid from seeping into the control panel.
Clean the condensate collector weekly.
Do not use chlorine-containing disinfectants that may corrode metal parts.
- When should the seal be replaced?
Replacement is required if: visible cracks, deformation, or seal failure (e.g., A4 paper can be easily pulled out). Regular replacement every two years is recommended.
- How do I determine if descaling is necessary?
Descaling is required if the heating time is increased by more than 30%, the steam generator makes unusual noises, or the temperature fluctuates significantly.
Equipment Management Issues
- How long should sterilization records be kept?
Physical monitoring records should be kept for at least three years, biological monitoring records should be kept permanently, and electronic data should be backed up twice.
- How should equipment be stored when not in use for an extended period?
Drain the water tank, dry the interior, apply silicone grease to the seals, and run the self-test program once a month.
- Which instruments cannot be sterilized at high temperatures?
Precision electronic devices (such as endoscopes)
Plastic products (melting point below 121°C)
Battery-powered equipment
Special Issues
- Is white powder appearing on instruments after sterilization?
This is due to mineral deposits caused by hard water. A pure water system should be installed. Contaminated instruments should be wiped with sterile gauze dipped in distilled water.
- What are the emergency measures for deteriorated door seals?
Cracks can be temporarily filled with medical silicone, but the original seals should be replaced as soon as possible and tested for airtightness.
- What should I do if the equipment alarm indicates "abnormal water level"? Check: whether
the water inlet valve is open, whether the filter is blocked, whether the water level sensor is faulty, and manually add water if necessary.
 EN
EN
 English
English 中文简体
中文简体
.png)